Kevin Rosin Eye Care New York
Monday, March 23, 2015
Scleral Contact lens fitting for the challenging patient
Scleral contacts are large gas permeable (breathable) contact lenses specially designed to vault over the entire cornea and rest on the "white" of the eye (sclera). Scleral lenses functionally replace the irregular cornea with a perfectly smooth optical surface to correct vision problems caused by keratoconus and other corneal irregularities or anomalies. The space between the cornea and the back surface of a scleral lens acts as a fluid reservoir to fill in any irregularity and to provide comfort for people with severe dry eyes who otherwise could not tolerate contact lens wear.
Scleral contacts are significantly larger than standard gas permeable (GP) contacts and have a diameter equal to or greater than that of soft contact lenses. The smallest sclerals are approximately 14.0 mm in diameter, and the larger can be up to 24 mm.
Lenses that are 18 mm or smaller are often sub-categorized as mini-sclerals.
Large-diameter scleral and semi-scleral GP lenses rest on the sclera and vault over the misshapen cornea in keratoconus.
The average human cornea is approximately 11.8 millimeters in diameter, so even the smallest scleral contacts are designed to cover the entire corneal surface.
In comparison, most conventional GP contact lenses are 9.0 to 9.5 mm in diameter and cover only 75 to 80 percent of the cornea.
Another category of gas permeable lenses bridges the size gap between conventional GP lenses and mini-sclerals. These lenses, called corneo-scleral lenses, generally are approximately 13 to 15 mm in diameter.
Corneo-scleral lenses often are a good choice for people who require larger-than-normal GP lenses for greater comfort. They also are frequently used when contact lenses are needed after LASIK or other corneal refractive surgery to correct irregular astigmatism.
The size of lens used often is determined by the degree of complexity of the condition. Milder forms of keratoconus and irregular astigmatism from corneal grafts and refractive surgery often are easily managed with scleral lenses at the smaller end of the spectrum.
Smaller scleral and mini-scleral contacts can be easier to apply, can be less costly and require fewer care products.
More complex conditions, including advanced keratoconus, pathologically dry eyes or severe ocular surface disease that might require a large tear reservoir, often are fitted with larger scleral lenses, as they have more capacity to hold fluid or bridge large changes in corneal curvature.
Many optometrists and ophthalmologists recommend scleral contact lenses for a variety of hard-to-fit eyes, including eyes with keratoconus.
In cases of early keratoconus, a standard GP lens may be used. However, if the lens does not center properly on the eye or moves excessively with blinks and causes discomfort, switching to a large-diameter scleral contact lens may solve the problem.
Because scleral lenses are designed to vault the corneal surface and rest on the less sensitive surface of the sclera, these lenses often are more comfortable for a person with keratoconus. Also, scleral lenses are designed to fit with little or no lens movement during blinks, making them more stable on the eye, compared with traditional corneal gas permeable lenses.
In addition to keratoconus, scleral contact lenses can be used for eyes that have undergone a cornea transplant, and for people with severe dry eyes caused by conditions such as Sjogren's syndrome, graft-versus-host disease (GVHD) and Stevens-Johnson syndrome.
Advances in lens design technology are allowing manufacturers to design scleral lenses that can correct more conditions than ever before, including bifocal sclerals for the correction of presbyopia.
Scleral contact lenses are custom-made for each wearer, so fitting scleral contacts demands greater expertise and more time than fitting standard soft or GP contact lenses.
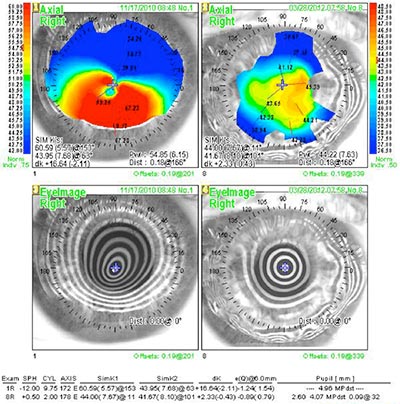
Often, computerized maps of the curvature of the entire cornea are generated to facilitate the lens fitting, and several trial lenses of different sizes and curvatures may be applied to the eye during the fitting process.
Also, depending on the complexity of the problem and how the individual eye tolerates the scleral lens, adjustments of lens parameters may be needed, which will require additional lenses to be made and exchanged. The entire scleral lens fitting process can take several visits to determine the optimal lens for each eye.
We have had extensive experience here at Farkas, Kassalow, Resnick and Associates. Feel free to call to set up a consultation or for any further information you require.
Dr. Kevin D.Rosin
212-355-5145
www.eyewise.com
Monday, March 9, 2015
Keratoconus - Custom Contact Lens Evaluation and Fitting
Keratoconus is an irregularity of the cornea (front of the eye) which usually leads to visual distortion and blurred vision. Most commonly a significant amount of astigmatism is found and Keratoconus patients tend to see significantly better in contact lenses as apposed to glasses.
Previously, patients with Keratoconus relied on Hard/Rigid contact lenses for functional vision. Although this is still the more common route, patients with corneal anomilies or injuries have a wide array of choices such as soft lenses specificaly designed for Kerataconus such as the Novakone lens, hybrid lenses which are hard (gas permeable) in the centre and soft on the outside such as the Synergeyes and Ultrahealth lenses, Sclereal and minis scleral lenses which are large but often comfortable and cornea protective and being fitted with increasing frequency in addition to piggybacking which includes a Kerataconus hard lens sitting on top of a soft lens adding to comfort , wearability and stability.
Keratoconus is usually picked up during a comprehensive eye examination. Keratometry and Corneal Topography are the gold standards of assessing and evaluating Keratoconus and corneal irregularities. Topography is digital corneal imaging using a device that analyzes the corneal shape. Another test we perform is called pachymetry, measuring corneal thickness which is usually thin in patients wth Keratoconus.
We, the Doctors at Drs. Farkas, Kassalow, Resnick and Associates, P.C. (www.eyewise.com) have been specializing in the contact lens management of Keratoconus (KC) for more than three decades, Having more than 90 years of collective experience. We have many designs available and thousands of lenses on site streamlining and often shortening the fitting process. We have most lens designs at our disposal and with experience, patience and expertise do all we can to make it a comfortable and pleasant sight enhancing experience.
Please feel free to contact me, Dr.Kevin Rosin for any further information and contact our office 212-355-5145 to schedule a consultation and to find out what are the best contact lens options for you.
Sincerely,
Dr. Kevin D. Rosin
212-355-5145
30 East 60th St., Suite 201
New York, NY 10025
www.eyewise.com
Roslyn, LI office at 516-365-4500
What exactly is Keratoconus?
Keratoconus is a condition in which the normally round, dome-like cornea (the clear front window of the eye) becomes thin and develops a cone-like bulge. Keratoconus literally means “cone-shaped cornea.” KC is a degenerative condition and scar tissue may eventually develop. KC Results in significant visual impairment.
The reported prevalence of KC varies widely depending upon the geographic location, diagnostic criteria used, and the cohort of patients selected. It ranges from 0.0003% to 2.3%. Keratoconus affects both genders fairly equally, although some investigators report a slightly greater incidence in males.
How did I get Keratoconus?
The underlying reason for its development has not been definitively identified and is currently the topic of much research.
Most likely the cause is due to more than one factor. The path that leads to the thinning of the cornea may start with a "trigger", followed by a cascade of events in the eye tissues. The primary trigger is not known. Possible factors include hormonal changes in the patient, genetic predisposition to altered inflammatory mediators and/or their receptors in the patient's cornea, or a pattern of eye-rubbing or poor fitting RGP lenses.
What symptoms are common in Keratoconus?
Keratoconus usually affects both eyes, though symptoms in each eye may differ. Symptoms usually start to occur in people who are in their late teens and early 20s and may include:
• Blurring of vision
• Distortion of vision
• Increased sensitivity to light
• Glare
• Mild eye irritation
The most commonly reported complaint leading to a diagnosis of keratoconus is reduced clarity of vision despite recent and multiple prescription changes.
Will my KC progress and, if so, how quickly?
Keratoconus affects all patients differently but there are some commonalities in the natural history of the condition. In the earliest stages, slight blurring, distortion of vision, and increased sensitivity to glare and light occur. Symptoms usually first appear in the late teens and early twenties. The average age of onset is 16, but onset as young as 6 yrs. has been recorded. KC may progress for 10-20 years and then slow in its progression. KC rarely develops after age 40. It may halt at any stage from mild to severe and each eye may be affected differently. The disease develops asymmetrically; one eye is usually more advanced at the time of initial diagnosis. Patients may endure discomfort and reduced vision over a long period of time.
Is there anything I can do to help stop my KC from progressing?
While there are no conclusive studies, we recommend that you avoid vigorous eye rubbing as there is some anecdotal evidence that this may be associated with progression. Keratoconus may be worsened by overexposure to sunlight, improperly fitting contacts, and chronic eye irritation.
Will my children get Keratoconus?
While scientific-based evidence supports a role for genetic factors, this does not mean that if you have a child with keratoconus the child will necessarily develop the disease. Only 13–15% of keratoconus patients have a family history of keratoconus. Given that genes do play a role in its development, in order to provide a medical cure, the genes that contribute to the development of keratoconus have to be identified and either replaced or suppressed. This is the only potential hope for a permanent cure to stop progression of keratoconus and ensure the cornea will no longer continue to thin. Research is ongoing in this area.
I was told I need hard contact lenses to stop my Keratoconus from progressing; is this true?
Contact lenses for KC are intended to correct the optical distortion caused by the corneal “bulge”. The conical shaped cornea causes irregular astigmatism which, when present in more than a mild amount, is not correctable by ordinary eyeglasses. Contact lenses, which rest directly on the surface of the cornea, smooth the optical surface and, for this reason, correct the irregular astigmatism and restore vision to more normal levels. Contact lenses are not intended nor will they stop the progression of the disease. Well fitted lenses will vault the cornea to reduce the possibility of scarring; they are not intended to press or have a “girdle” effect. Many patients will experience a temporary improvement in vision after they remove their contact lenses. This effect is due to a temporary “molding” of the cornea. The effect may last anywhere from a few minutes to several hours, but it is not permanent.
Do I absolutely have to wear contact lenses?
In the very early stages of KC or in very mild cases, contact lenses are often not necessary. This varies by patient and is determined by the patient’s visual sensitivity to blur as well as how critical their vision is to their daily personal and occupational needs. Contact lenses usually become necessary when the astigmatism increases to greater than 4 Diopters. With prescriptions below that level, many patients continue to do well without any form of correction or with conventional spectacle correction. Routine reevaluations are recommended as per the advice of your eye care professional or sooner, if you notice any changes in vision.
What kinds of contact lenses are available to manage Keratoconus?
There have been significant advances in the contact lens management of KC over the past decade and product development continues to offer more options. The newest lens technologies allow us to deliver unprecedented levels of visual clarity and comfort to patients in every phase of the disease.
For patients with very mild to moderate disease, expanded parameters in soft lens materials offer an excellent option. Some patients who achieve less than acceptable vision in these standard designs will, instead, do very well in custom soft lenses. These KC design soft lenses are slightly thicker than their conventional counterparts. This increased thickness allows for better masking of the optical distortions.
Custom Soft Lens for Keratoconus
Hybrid lenses (a fusion of a rigid lens center and soft lens skirt) are now available in highly oxygen permeable materials and are often ideal for moderate KC. The rigid lens center corrects the irregular astigmatism and the soft lens skirt delivers improved comfort.
Rigid gas permeable lenses, the traditional and previously “only” way to correct KC are now available in larger diameters and are fully customizable. They offer the best option for the more advanced cases. Oftentimes, comfort is brought to even higher levels by utilizing a “piggy-back” approach. Piggy-backing involves inserting a thin, highly oxygen permeable soft lens first and then layering the rigid lens on top. This system is appropriate for just about any corneal shape and condition.
Piggy Backed Contact Lenses
The newest entry into the contact lens arena for KC is the Scleral Contact Lens. These are very large gas permeable lenses that work best for very advanced cases. They are quite comfortable and there is no risk of the lens dislodging.
Because KC is a complex disease, the fitting of contact lenses is complex as well. It can take anywhere from one month to several months. Routine re-evaluations are typically conducted two to four times per year.
What are my chances of needing a corneal transplant?
Only 15-20% of those with keratoconus ultimately require corneal transplant surgery. A corneal transplant is warranted when the cornea becomes dangerously thin or when sufficient visual acuity to meet the individual’s needs can no longer be achieved by contact lenses due to steepening of the cornea, scaring or lens intolerance. Lens intolerance occurs when the steepened, irregular cornea can no longer be fitted with a contact lens, or the patient cannot tolerate the lens. It is important to understand that even after a corneal transplant, most patients will likely still require a contact lens. The purpose of the surgery is to restore a clear, less irregular, unscarred “window”. The shape of the cornea after the surgery will still be somewhat irregular, requiring a specialty fitting. Therefore, corneal transplants are usually a “last resort”. In some cases, however, patients may achieve acceptable vision with regular eyeglasses post corneal transplant surgery.
Are there any other treatments available for Keratoconus?
Other options for managing Keratoconus include Intracorneal Rings, commonly known as INTACS and Corneal Collagen Crosslinking (CXL). These can be done alone or in combination with each other and with contact lenses.
Intacs are thin plastic, semi-circular rings inserted into the mid layer of the cornea. When inserted in the keratoconus cornea they flatten the cornea, changing the shape and location of the cone. The placement of Intacs remodels and reinforces the cornea, eliminating some or all of the irregularities caused by keratoconus in order to provide improved vision. Eyeglasses or contact lenses are still additionally necessary for most patients to achieve functional vision.
Corneal Collagen Crosslinking with Riboflavin (CXL) is a developing keratoconus treatment. CXL works by increasing collagen crosslinks within the cornea. Collagen crosslinks form the natural framework of the cornea and they are what give the cornea the structural support and mechanical integrity. Natural corneal crosslinking occurs through our normal exposure to sunlight, which is thought to be one reason why keratoconus does not progress after the fourth decade of life. CXL is a very safe procedure and is currently undergoing clinical trials here in the U.S. It has been performed abroad for several years and the results have been extremely favorable, with very little risk. CXL is a procedure that can arrest the progression of KC, but cannot reverse it to a significant degree. Glasses and or/contact lenses still remain necessary for functional vision in patients who required them before the procedure. For young patients, newly diagnosed, who have reasonably good visual acuity, CXL may offer the benefit of reducing the possibility of requiring stronger glasses or contact lenses in the future.
What is involved in a contact lens fitting for KC?
Your first visit, called the consultation visit will last roughly one hour.
At this visit, we will analyze your cornea and all aspects of the front surface of your eye, including your tears and your lids. We will also make a determination of the severity of your KC including your astigmatism and other aspects of your prescription.
The second visit, called the diagnostic evaluation (which is often conducted on the same day and consecutively to the consultation) involves determining which type or types of contact lenses will best be suited to your particular corneal shape and visual needs. One or more types of contact lenses will be tried while you are in the office. At the conclusion of the this process (usually lasting one hour), we will have the information necessary to design and order your initial pair of contact lenses. An appointment will then be scheduled for you to return approximately 10 days later for the dispensing visit.
At the dispensing visit (approximately 45 min.) your lenses will be inserted and, after settling, will be checked by the doctor. You will then be instructed on insertion and removal and lens care with one of our expert technicians. You will be given a wearing schedule to safely adapt to lens wear and will be appointed a follow-up visit for one week.
Your follow-up visit will last approximately 30 min. Your progress will be analyzed by the doctor and any lens necessary treatment or lens design changes will be made. Routine follow-up visits are conducted on an on-going basis according to your individual case. During the initial fitting period (first 90 days) lens exchanges will be made as necessary and you will likely be monitored for 3 visits. Thereafter, quarterly or semi-annual visits are recommended.
For more detailed information regarding our specialized services for Kerataconus and other ocular conditions please visit us at www.eyewise.com
astimatism, contact lenses, cornea, corneal irregularity, distorted vision, distortion, ectasia, rubbing, Keratoconus, scleral lens, intacs, corneal transplant, rejection, topography, Novakone, Synergeyes, Ultrahealth, Kerasoft, topography, comfort, tearing,
Monday, November 10, 2014
Blue Blocking Lenses for Healthier Eyes
We have all grown up knowing the importance of sun protection for both our eyes and our skin and many of us take action with both sun screen, sunglasses, hats etc., but we are now in a new age where much of our time is spent under compact fluorescent light bulbs, either in front of a computer an I-Pad (or other tablet) or a Smartphone.
Besides the amount of eyestrain these devices place on our eyes and our visual system, lots of new research is showing that these devices also give off a form of blue light radiation that appears harmful to our eyes and may increase our risk of Cataracts and Macular degeneration in addition to exacerbating dry eyes.
SELECTIVELY FILTERS HARMFUL LIGHT
Blue-violet light is present everywhere
•OUTDOORS: Blue-Violet light is emitted all year round in any weather (sunny, cloudy, rainy, etc). This is even true when the light comes through windows in your home, office or car.
•INDOORS: Blue-Violet light is also present throughout the day and night. It is emitted from computers, tablets, most smartphones and compact fluorescent light bulbs.
There are now new lens coating technologies available for glasses that can help protect our eyes, in addition to minimizing eyestrain and maximizing visual comfort.
Please contact me Dr. Kevin Rosin for further information and for examination to find out what lens and eye care options are best for you.
Tel: 212-355-5145
Dr. Kevin Rosin
together with Dr.'s Barry Farkas, Jordan Kassalow, Susan Resnick and Regina Zyszowski
30 East 60th St.
New York, NY 10025
Tuesday, October 29, 2013
Miru 1 Day Contact Lens - Ultrathin Flat Pack
As part of our practice to bring innovation, quality and optimal vision we are in the process of helping launch a revolutionary new daily disposable contact lens in the US and our patients are to be among the first to try it, ahead of the national launch that will take place next year.
Our exciting new product is called Miru 1day, and it comes in an ultra slim package, barely 1mm thick. Besides being a very convenient product to carry around and store, it was designed to be easy to open, spill proof, and clearly a single-use device. An additional and very important feature is that the lens is always oriented with the posterior surface of the lens facing down, allowing the lens to be inserted without ever touching the part that will come into contact with the cornea.
Miru 1 Day
Miru 1day is made of hioxifilcon A, a HEMA-GMA soft lens polymer with 57% water content and excellent water retention properties aiding in comfort and minimizing dryness. The lens features aspheric optics for optimal vision and a comfortable edge .
The Miru 1day lens will be available from our unique Miru WebStore where patients can purchase their lenses online. If you would like to try out these amazing lenses call 212-355-5145 to set up an appointment.
Dr. Kevin Rosin
with Drs. Farkas, Kassalow, Resnick and Regina
30 East 60th St., Suite 201
New York,
NY 10025
www.eyewise.com
To learn about this innovative new product, we invite you to visit the Miru informational websites:
http://www.meniconamerica.com/consumer/features
http://www.meniconamerica.com/consumer/miru
Thursday, May 2, 2013
DRY EYE - Treat the Cause!
Lipiflow in the treatment of Dry Eye --- soon to be highlighted on the hit TV show 'The Doctors'
Being the first Eye Care practice in New York to use both the Lipiview and Lipiflow technology (since 2011) has not only led us to best understand this incredible analysis and treatment technology, but has allowed us to help and change the lives of countless patients suffering with meibomian gland dysfunction and dry eye disease.
Most dry eye patients with inflamed and/or blocked meibomian (oil secreting eyelid glands) would be good candidates for the procedure and this can easily be assessed and measured in office.
The treatment, if appropriate for you, helps prevent the evaporation of your tears, improves tear quality and thus keep good tears on the eyes surface for longer, aiding in decreasing associated inflammation, ultimately decreasing dryness and burning symptoms.
Dry eye disease is an extremely common and sometimes debilitating condition affecting approximately 28 million Americans. Up to 80% of dry eye disease is as a result of evaporative dry eye known as meibomian gland dysfunction (MGD).
We here at Farkas, Kassalow, Resnick and Associates have had great success with the Lipiflow and have seen amazing improvements in both signs and symptoms with prolonged benefits in most patients. Patients report much improved comfort and we see significant clinical improvements related to their eyes and eyelids.
Lipiflow thermal pulsation offers a simple, quick, easy, safe, painless treatment solution for evaporative dry eye and has been shown to be significantly (2-3x) more effective then 10 minutes of diligent, warm compresses and lid massage done daily for several months.
LipiFlow is designed to treat the root cause of Evaporative Dry Eye, blocked Meibomian glands. Opening and clearing these blocked glands can allow them to resume natural production of lipids (oils) needed for a healthy tear film.
Remember to watch the TV show 'The Doctors' most likely being aired on May 6th, 2013 covering this innovative and novel solution to evaporative dry eye.
Please feel free to call me Dr. Kevin Rosin @ 212-355-5145 or my colleagues, Dr's Barry Farks, Jordan Kassalow, Susan Resnick and Regina Zyskowski or email me at doctors@eyewise.com with any other questions. If this is something you want to explore further it would be our pleasure to have you come in for an evaluation and to help manage this frustrating, uncomfortable and often painful condition.
Dr. Kevin Rosin
212-355-5145
30 East 60th St.
Suite 201
New York, NY
Visit www.lipiflow.blogspot.com for more info on Lipiflow in the treatment of meibomian gland dysfunction

Monday, April 29, 2013
RED AND ITCHY EYES
After a long winter and a delayed spring, Allergists are expecting a "rough" allergy season this spring and summer. We are already seeing lots of symptomatic patients complaining of itching, watering, red uncomfortable eyes often more severe than years past.
It is imperative that you have your eye doctor examine you to differentiate between allergies and other types of eye infections (such as viral conjunctivitis) and eye conditions as often there can be similiar symptoms among various maladies.
Oral allergy medications such as Zyrtec and Clarityn are often not enough to control and alleviate ocular allergy symptoms and in many cases may result in or add to dryness of the eyes.
An eye drop is usually needed when eyes are affected by allergies and there are some eye drops that can also prevent symptoms from occuring if started early enough. These drops have antihistamine properties (reduce or eliminate itching and redness) and are mast cell stabilizers which prevent the eyes from reacting to allergens in the environment. Drops like Pataday, Lastacaft, Bepreve, Elestat, Optivar among others fall into this category and also have different dosing and side effects so it is best to consult with your doctor before using. In more severe cases steroid eydrops are often very helpful in bringing relief and eliminating symptoms. Using these drops prior to the onset of symptoms can help prevent and ultimately decrease the overall severity of the allergic symptoms.
I often tell my patients to refrigerate their unpreseved artificial tears and they love the cooling soothing effect this brings about in addition to decreasing redness and flushing out or diluting the eye allergens.
Dry eyes also can result in greater and more exagerated symptoms and it is therefor imperative to have this managed by your eye doctor as well.
Should you have any questions please feel free to email me, Doctor Kevin Rosin at eyedockev@yahoo.com. Together with Doctors Barry Farkas, Jordan Kassalow, Susan Resnick and Regina Zyskowski we focus on Dry Eye , contact lenses and Ocular Allergies.
Visit us at our website www.eyewise.com or call me at 212-355-5145
Thursday, February 23, 2012
DryEyeTreatmentLipiflow
Dry Eye Treatment- combating Meibomian Gland Dysfunction - Lipiflow Thermal Pulsation
'Meibomitis' or Posterior Blepharitis - A new buzz word in eye-care but an old chronic annoying condition.
Eye Doctors - Optometrists and Ophthalmologists have been taking care of dry eye related conditions often caused by meibomian gland dysfunction (reported in up to 65% of cases)for many decades. Blepharitis has also been reported in as many as 47% of patients presenting to the eye doctor.
Meibomitis is as a result of blocked meibomian glands which line the eyelids just behind the eyelashes. These glands are responsible for secreting oil into the tears and preventing evaporation of the Aqueous (watery)layer of the tears therefore keeping the tears on the surface of the eyes for longer, between blinks.
Treatment has routinely included warm compresses with eyelid massage, in addition to eye drops, supplements (fish oils) and oral medication (Doxycycline).
The mainstay management utilizing the warm compresses has come with poor patient compliance and thus varying and often undesirable results leading to a deterioration in the condition and thus worsening of Dry eye and its symptoms.
A new and dynamic therapy called 'Lipiflow thermal pulsation' has recently become commercially available and prior clinical studies have shown impressive results and amazing patient testimonials.
We, at the eye care practice of Dr's. Farkas, Kassalow, Resnick and Associates have been fortunate to be the first practice in New York to use this amazing treatment, and over the past several months have seen many happy and successful patients treated with the Lipiflow treatment. It is very exciting to finally have a treatment for this chronic and often cumbersome condition that does not require daily involvement from the patient and may keep them free from eye medications as well. Studies have shown patients reporting a reduction in there dry eye symptoms, often in excess of a year and this has been mirrored by the clinical objective findings too.
Lipiflow works by applying energy to the affected glands with warmth to the back eyelids and gentle pressure to the front of the eyelid. The procedure takes less than fifteen minutes and is well tolerated.
We also use a new and revolutionary tool called the Lipiview ocular surface interferometer to analyze the lipid (oil) layer of the tears obtaining an objective and repeatable quantification of ones tear stability, giving us more critical information in assessing Dry eye disease and its management.
Please do not hesitate to call me, Dr. Kevin Rosin @ 212-355-5145 or email me at doctors@eyewise.com should you need any other information. You can also go to http://www.tearscience.com/en/ to get information on the Lipiflow treatment and the Lipiview system.
www.eyewise.com
Kevin Rosin in association with Dr's Farkas kassalow & Resnick
Tel: 212-355-5145
30 East 60th St, Suite 201 New York, NY